Pressure Toxicity: When the Cure Becomes the Complication
~ ~ ~ ~ ~
15 May 2025
By David E. McCarty, MD, FAASM (but you can call me Dave)
~ ~ ~ ~ ~
Introduction: Welcome Back to the Isle
The wind was high that morning on the Isle of Sleep Apnea (get it? It’s a Dad Joke! I LOVE SLEEP APNEA…tee hee!) and Claudio Mahoney, ever the cheerful explorer with his trusty Yellow Smiley shirt and his two blonde cowlicks bouncing in opposition, clutched his nasal pillows with a growing sense of dread. Something wasn’t right. His dreams were still broken. His mouth tasted like cardboard. His sleep-wake complaints, those rascal seagulls, still circled his consciousness, cawing.
"I'm doing everything right," Claudio muttered. "Compliance over 90%. AHI is technically fine. And yet... I feel like I've been steamrolled by a freight train of invisible pressure."
From the tall grass, Ishmael Trodglampin appeared, carrying a mug of the Coffee Hut's strongest brew. He wore his poet's cap askew and narrowed his one good eye. "Ah, dear Claudio," he said, sipping. "It sounds like you’ve met our old frenemy... pressure toxicity."
Truth can be stranger than fiction!!
~ ~ ~ ~ ~
The Seductive Simplicity of “APAP 5-20 cmH2O, choose P90”
Auto-titrating CPAP (APAP) has revolutionized therapy delivery in sleep medicine. It is intuitive, flexible, and easily deployed. Devices like ResMed's AirSense series promise to "find the right pressure for you" by analyzing breath-by-breath parameters. And yet, like so many enchanted gifts in ancient folklore, there’s a catch.
The default starting range of 5-20 cm H2O has become the standard configuration across many DME channels, with the assumption that the machine will gently and intelligently select an optimal pressure. Unfortunately, the use of the 95th percentile pressure as a titration target has led to the widespread unintentional practice of over-pressurization. The logic goes something like this: "If a patient spends 5% of the night at 14 cmH2O, then 14 is probably the right number."
It is not.
In fact, such a strategy can unleash a cascade of physiological problems that are well-known in the clinical trenches but poorly represented in formal literature. These include:
· Oral air leaks and resultant dry mouth
· Disrupted sleep due to pressure intolerance
· Increased expiratory effort and central events
· Premature escalation to oronasal masks
· Mouth-breathing and its impact on upper airway tone and nasal disuse
This collection of maladies is what we here on the ISLE call “Pressure Toxicity.” We made a whole PODCAST EPISODE about it last Halloween, calling it THREE TALES OF TERROR!
~ ~ ~ ~ ~
Pressure Toxicity: A Clinical Syndrome with No ICD Code
Pressure toxicity is not a disease. It is a pattern. A phenotype. A recognizable syndrome of maladaptation that arises when therapeutic pressure exceeds patient tolerance or anatomical necessity. In the narrative of empowered sleep apnea care, pressure toxicity is a villain born not of intention, but of assumption.
The origins of this syndrome lie in a cultural mismatch: industrialized respiratory support delivered in a population that often requires nuanced, hand-tailored care. The concept was born from countless anecdotes and case studies of patients who dutifully followed their therapy plan and yet found themselves deteriorating. They arrived at the clinic with complaints of air hunger, mask rejection, and cognitive fog, only to be met with "But your AHI is excellent!"
This advertisement was brought to you by a grant from Doctors Against Disempowered Decision-Making (D.A.D.D.)
~ ~ ~ ~ ~
The Evidence (and the Silence) in the Literature
While the term "pressure toxicity" has yet to achieve recognition in the academic canon (here we come, ivory tower!!), the complications it describes are known to sleep medicine. A study by Massie and Hart in 2003 documented that leaks and discomfort are major reasons for poor adherence in CPAP therapy.[1] The well-known SERVE-HF trial, though centered on heart failure, exposed the sobering reality that positive airway pressure is not inherently benign.[2]
More recent work by Ayas and colleagues highlights the problem of high-pressure intolerance in real-world practice.[3] Interestingly, the current ResMed AirSense algorithms do include parameters to reduce pressure when leak is detected, but these are often insufficient to overcome structural problems (e.g., mouth breathing, malocclusion, or anatomical resistance).
Yet, the common rollout of 5-20 cmH2O persists. Why?
Partly, it is operational convenience. DME workflows favor standardization. APAP is thought to be "set it and forget it." Pressure complaints are dismissed as outliers, and the 95th percentile pressure is misused as a titration metric despite guidelines from the AASM that advise against this practice in isolation.[4]
~ ~ ~ ~ ~
From Nasal to Oronasal: The Domino Effect
Pressure toxicity often initiates a shift from nasal CPAP to oronasal masks, which then fosters mouth breathing. This behavioral shift, in turn, promotes nasal disuse syndrome—leading to more congestion, more leak, and higher pressure demands. The vicious cycle completes itself, and the patient is labeled "non-compliant" when they ultimately abandon therapy.
The literature is increasingly clear: oronasal masks are associated with higher leak rates, reduced adherence, and lower satisfaction scores compared to nasal interfaces.[5] Yet patients are routinely escalated to them early in therapy due to mismanaged leak and pressure intolerance.
~ ~ ~ ~ ~
A Better Way: Titration by Humanity
In Empowered Sleep Apnea, we recommend an alternative: Start low. Go slow. Mind the nose.
Instead of 5-20, consider an initial range of 5-8 or 6-10 cmH2O. Optimize nasal patency. Use heated humidification. Introduce expiratory pressure relief (e.g., EPR = 3 on ResMed) judiciously. Follow up within 1-2 weeks with data and conversation.
Pressure, like medication, is a dose. And every dose needs a therapeutic window.
What is required now is a cultural shift. One that views PAP not merely as technology, but as an interface between biology and behavior. We must retire the myth of "set it and forget it" and embrace instead the mindset of respiratory coaching. Our aim isn’t to “get a patient compliant” on CPAP, but to help restore effortless naso-diaphragmatic breathing, during Wake and Sleep.
~ ~ ~ ~ ~
Looking Forward: The Research We Need
It is time to formally study pressure toxicity as a syndrome. Proposed research directions:
1. Longitudinal outcomes comparing high-range APAP (5-20) vs low-range APAP (5-10) on adherence, leak, and sleep quality
2. Studies correlating 95th percentile pressure vs therapeutic efficacy across different phenotypes
3. Trials evaluating interface progression pathways (nasal → oronasal vs nasal with troubleshooting)
4. Patient-reported outcomes in those with high-pressure intolerance
Moreover, it may be time for a new scoring metric: not just AHI, but a Pressure Tolerance Index (PTI) that reflects the biotolerability of the selected therapy.
~ ~ ~ ~ ~
Conclusion: Naming the Thing That Hurts Us
As Claudio finishes his coffee and looks out over the cliffs of the Isle, Ishmael puts a hand on his shoulder.
"Pressure isn't evil," he says. "But it's powerful. And anything powerful, dear friend, must be respected."
We do not need to abandon APAP. We need to reclaim it.
Not as a blind prescription, but as a conversation. Not as a mandate, but as a map. And maybe, just maybe, if we take the time to listen, we can help more Claudios find their way back to Pleasant Dreams Beach.
The Air B&B of our dreams :) :) :)
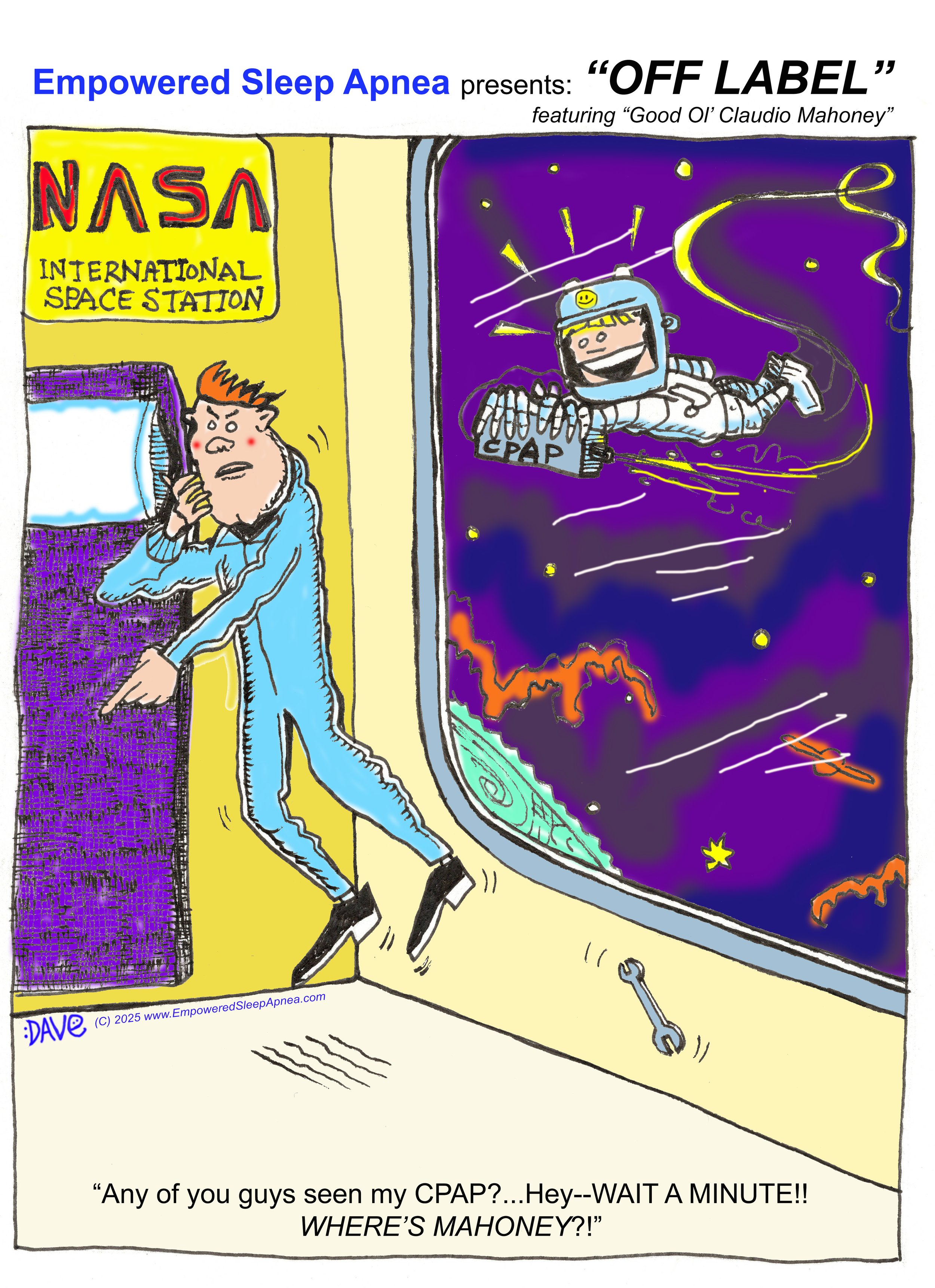
When positive airway pressure is set “too high”, it’s a common report that it “feels like a jet engine” strapped to one’s face. I decided to have some fun with the Jet Engine image with this cartoon…and YES I know there is no air in space…I bet Claudio rigged that machine up with pressurized gas!! LOL!
This Cartoon originally appeared in SLEEP REVIEW magazine, April 2025 Edition…
References
1. Massie CA, Hart RW. Clinical outcomes related to the use of auto-titrating CPAP. Chest. 2003;123(2): 414-420.
2. Cowie MR, Woehrle H, Wegscheider K, et al. Adaptive servo-ventilation for central sleep apnea in systolic heart failure. N Engl J Med. 2015;373:1095-1105.
3. Ayas NT, Hirsch Allen AJ, et al. Adherence to continuous positive airway pressure therapy in patients with obstructive sleep apnea. Can Med Assoc J. 2020;192(29):E827-E837.
4. Berry RB, Kryger MH, Massie CA. AASM Scoring Manual Version 2.6. Darien, IL: American Academy of Sleep Medicine; 2020.
5. Borel JC, Tamisier R, Wuyam B, et al. Oronasal mask leaks during CPAP: a systematic review of their impact on treatment efficacy. Sleep Med Rev. 2013;17(2): 91-100.