When “Normal” isn’t NORMAL: The Trauma of Dismissal
By David E McCarty MD FAASM (but you can call me Dave)
21 May 2025
~ ~ ~ ~ ~
“If you are silent about your pain, they’ll kill you and say you enjoyed it.”
— Zora Neale Hurston
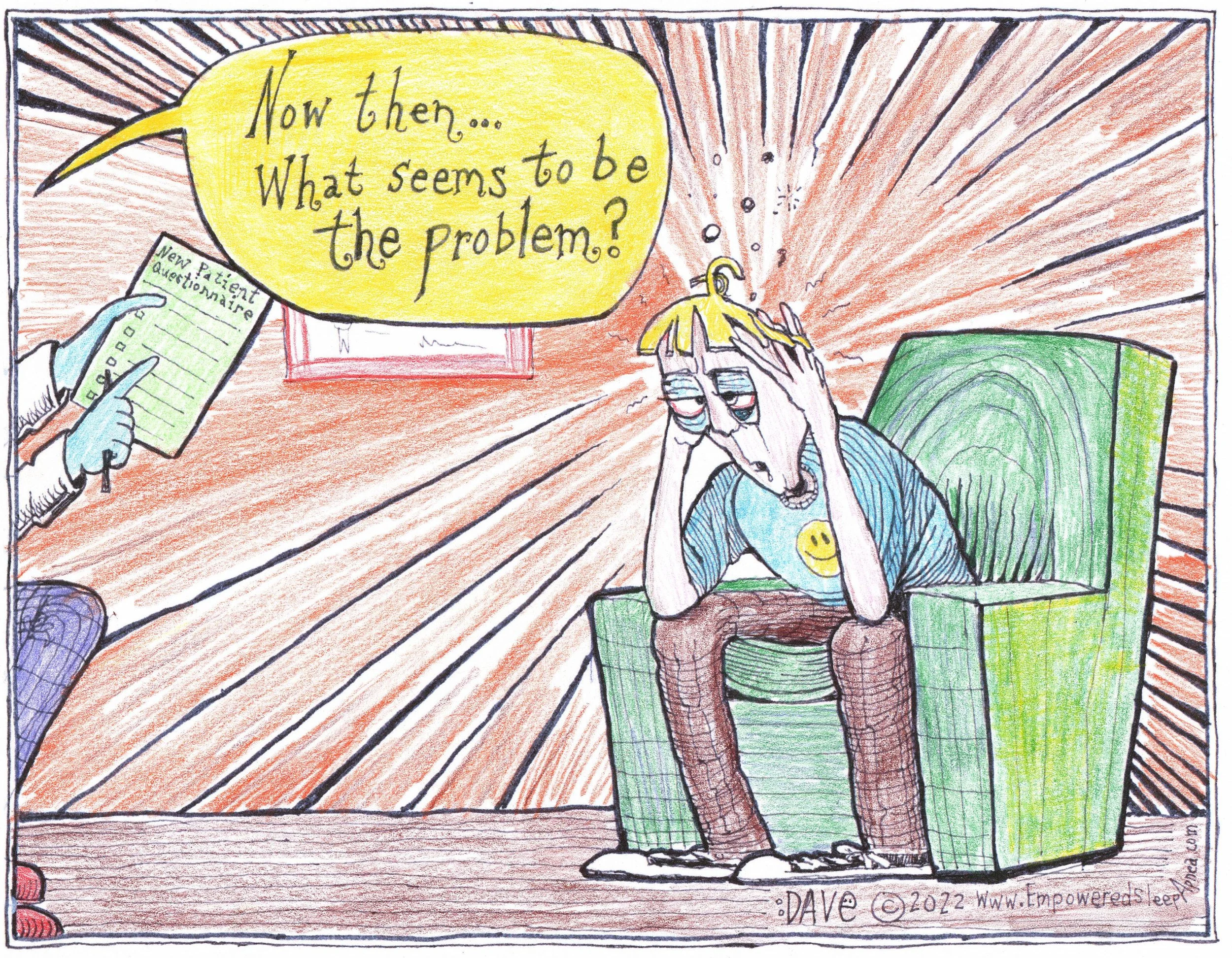
Imagine this: you drag yourself into a sleep clinic after months—maybe years—of feeling like you've been steamrolled by a Zamboni every morning. You're exhausted, foggy, irritable, and emotionally strung out like a banjo at a bluegrass festival. You finally get your sleep study, thinking salvation is near.
Then comes the verdict.
"Good news! You don't have Sleep Apnea!"
A pause. Your body tenses. You lean forward. "But I can't stay awake in afternoon meetings. I feel like I'm being waterboarded by my own body at night. I dream in Morse code."
The PA smiles sympathetically and shrugs. "Your insurance won't cover treatment unless your apnea-hypopnea index is at least five."
And just like that, the curtain falls. The diagnosis is boxed up, labeled "normal," and shipped to the Island of Misfit Symptoms, and you’re left to mop up what’s left.
Welcome to the trauma of dismissal.
RERA-ly Recognized: The Quiet Tragedy
Let me tell you about the sneaky undercurrent in this story: RERAs (Respiratory Effort-Related Arousals). These are the ninja assassins of sleep architecture. They don’t cause the big dramatic O2 desaturations like apneas or hypopneas. No, they're subtle. They disturb your sleep just enough to yank you out of restorative phases, over and over again, without leaving bruises that show up on insurance paperwork.
According to the International Classification of Sleep Disorders (ICSD-3), you can be diagnosed with obstructive sleep apnea if your RDI (Respiratory Disturbance Index—which includes apneas, hypopneas, and RERAs) is over 5, and you have symptoms. Which you do. Boy, do you ever!
But many sleep labs have stopped scoring RERAs, because the American Academy of Sleep Medicine has made RERA-scoring optional for lab accreditation. And insurance? Many payors are stuck in the AHI-only world. If it ain’t apnea or hypopnea, it doesn’t count.
This, dear reader, is how people with real physiological dysfunction get told they’re “fine”, when the situation is far from it.
Gaslit by the Guidelines
If you're dismissed by your doctor because your AHI is "too low," the trauma isn’t just physical. It’s existential.
You start questioning your sanity. “Maybe I'm just lazy.” “Maybe I'm broken.” “Maybe I need more gratitude journaling and less complaining.”
You were ready to fight your condition. But now you’re fighting your reality.
This isn’t just bad medicine. It's a category error. It's what happens when insurance criteria are mistaken for clinical truth. When numbers replace narratives. When we swap out the complex, multicolored tapestry of human sleep for a grayscale spreadsheet column labeled "AHI."
~ ~ ~ ~ ~
It's Not “All In Your Head.” It's In Your Upper Airway.
Let me say this clearly, for the folks in the back:
A “normal” AHI does not mean your sleep is normal,
and it doesn’t guarantee that OSA is absent!
If you wake up feeling wrecked, and your study didn't even score RERAs, your physiology has been half-interpreted. We looked at the moon and only measured its craters, not its glow.
You may have RERA-predominant OSA. The Airway Focused Dentistry world is calling this entity Upper Airway Resistance Syndrome (UARS), though the American Academy of Sleep Medicine has officially retired this term, adding to the confusion. The fact that some insurance plans don’t recognize it doesn’t mean it’s not real. It means our tools (and our payors) are still catching up to your biology.
The Way Forward: Reclaiming Clinical Truth
So what do we do? We reclaim the art of interpretation so that we accurately capture the complexity of this problem, not just determine who will “qualify” for treatment.
Clinicians: Please stop telling patients they’re “fine” when they’re obviously not. Please stop pretending the 4% AHI is the North Star. It’s just a number. A helpful one, in some respects, but a deeply flawed one, when it comes to communicating nuance. Listen to your patients. If they’re drowning, don’t check the barometer. Throw them a life raft.
Patients: Trust your inner narrator. If your body is shouting for help, don’t let a spreadsheet whisper over it. Seek out sleep professionals who understand nuance, who’ll look beyond the 4%AHI, who’ll see YOU!
This isn’t just about sleep. It’s about dignity. About the right to have your suffering acknowledged. About not being gaslit by guidelines and coverage criteria.
Your story matters…the details about this diagnosis matter…
So, let’s have a collective HUZZAH for all y’all who approach this problem with more than just a checkbox, and tip our hats to those who embrace the complexity!
HUZZAH!!! HUZZAH!!! HUZZAH!!!
(crows caw in the distance…caw! … caw! … caw!)
Dave
David E McCarty MD, FAASM
Boulder Colorado, 21 May 2025
PS: EMPOWERMENT SAVES!!