THE THREE STARS OF EMPOWERMENT
Or: Why Shared Consciousness Is the Only Way Out of the ‘Fragmentiest Place on Earth’
By David E. McCarty, MD, FAASM
(but you can call me Dave)
12 January 2026
~ ~ ~ ~ ~
I must go down to the seas again, to the lonely sea and the sky,
And all I ask is a tall ship and a star to steer her by
John Masefield in: “Sea Fever.” Salt-Water Ballads, 1902.
~ ~ ~ ~ ~
‘All I need is a Happy E and THREE STARS to steer by…’
There are moments in a field’s life when progress no longer comes from better tools, tighter algorithms, or more impressive machines, but from agreement, from shared orientation. There comes a moment of collectively finally looking up at the same sky and admitting we’ve been navigating by different stars.
Sleep Medicine is standing in one of those moments right now.
We are not short on expertise. We are not short on technology. We are not even short on good intentions. What we ARE short on is a shared consciousness of complexity, the kind Gen. Stanley McChrystal described in his landmark book Team of Teams when he realized that modern problems can’t be solved by command-and-control hierarchies, only by teams who share the same picture of the battlefield and are field-empowered to act on it.
In our world, the battlefield is the human sleep–wake system, the casualties are patients lost between silos, and the missing piece is not effort, but alignment.
At Rebis, and within the Empowered Sleep Apnea project, we’ve come to believe something both radical and disarmingly simple:
If clinicians, patients, payers, and allied disciplines cannot agree on the answers to three foundational questions, then no amount of clinical brilliance will save us from fragmentation.
These are not rhetorical questions; they are not branding exercises; they are not philosophical indulgences.
We see them as operational necessities.
So, Life-Fans, let it be heretofore be known that these THREE QUESTIONS are the Three Stars of Empowerment--the stars we sail by.
The snappy subtext is that until we agree on their meaning, many of our providers and patients will keep circling the same reefs, wondering why so many people are running aground.
~ ~ ~ ~ ~
Presenting: OUR THREE STARS
Let me start here: the order of the THREE QUESTIONS matters. Knowledge builds on itself to become wisdom. Complexity doesn’t necessarily self-stack into meaningful piles.
So: the THREE QUESTIONS, in order, are:
1. What is Sleep Apnea? 2. What else could this be? 3. Why should we treat it?*
~ ~ ~ ~ ~
* Earlier versions of this work asked Why should we treat it? before asking What else could this be? Over discussions with my co-creator (ERS), it became clear that this order unintentionally mirrored the very top-down reflexes we were trying to escape. Once treatment justification enters the conversation—especially through the lens of RISK—curiosity tends to collapse and alternatives fade from view.
Reordering the questions was a deliberate correction. By fully exploring what Sleep Apnea is, and what else might be contributing to a person’s story before asking whether stabilization is worth pursuing, we protect humility, preserve curiosity, and restore patient agency. In complex systems, the sequence of questions is not cosmetic—it is ethical.
~ ~ ~ ~ ~
Three questions to unite us all! Everything else we do--every sleep study, every appliance, every CPAP prescription, every surgical consult, every therapy decision--depends on how these questions are answered.
Miss the order? Confusion follows.
Fake the answers? Trust erodes.
Skip any of them, and the system fractures.
Folks, the THREE STARS are not optional, but navigational.
Having said that, the first star is, like the Pleaides, hard to look at directly. To appreciate its nuance and beauty, you must look at it kinda askance...
So: what’s in a name, anyway? What is Sleep Apnea?
Cue time warp sound effects as we transport ourselves inside an idea, inside the language itself, to try to find MEANING…
~ ~ ~ ~ ~
Star One: What Is Sleep Apnea?
This is where everything gets uncomfortable, where jargon multiplies, where silos get deep.
The short answer? Sleep Apnea is more than you think it is! But, as usual, I’m getting ahead of myself, so let’s back up.
Truth be told, it’s tempting to rush past this question because it feels “settled.” After all, “Sleep Apnea” has diagnostic criteria, billing codes, practice parameters, and decades of literature behind it.
But here’s the uncomfortable truth:
If you ask this question to ten different providers in the Sleep/Airway space, you might get ten different versions, ten different spins, ten different interpretations of the answer!
See, here’s the thing, Life-Fans: We can agree on how to label it, we can agree on how to score it, we agree on how to bill for it.
But agreement on classification is not the same as agreement on MEANING.
Here’s why the language of the Empowered Sleep Apnea project starts with honesty:
Sleep Apnea is more than you think it is.
~ ~ ~ ~ ~
Two Words and the Doorway They Open
Let’s start with that two-word term “Sleep Apnea”. Here at THE ISLE, this term is a doorway… a word-combo we use when breathing becomes unstable during sleep in a way that matters to your health.
That’s it!
Sleep Apnea is: unstable breathing during sleep that’s causing problems.
Hold on! Jargon alert! “Apnea” means “not breathing,” doesn’t it? We all know by now that this problem is more nuanced than just stopping and starting breathing. It’s not so black & white—there are shades of GRAY!! It’s about INSTABILITY, man!
To make it more interesting, here’s one more thing: the instability we’re pointing at can arise from very different mechanisms, carry very different risks, and demand very different responses to achieve stability!
Let’s take a closer look *SHALL WE*?? :)…
~ ~ ~ ~ ~
The Two Flavors of Breathing Instability
See, anytime somebody with unstable breathing comes through the door, we have to be thinking about two different FLAVORS of instability that might be present:
Obstructive Sleep Apnea (OSA) — where the airway collapses or narrows despite respiratory effort. This is choking physiology. When severe and untreated, it carries a strong signal for long-term cardiovascular harm and premature mortality.
Central Sleep Apnea (CSA) — where the signal to breathe waxes and wanes. The airway may be open, but the rhythm is unstable. This physiology often affects sleep quality and daytime function, but — outside specific contexts like advanced heart failure or opioid toxicity — does not carry the same mortality signal as obstructive disease.
Here’s the thing: most people don’t have ONE or THE OTHER. Most folks have BOTH FLAVORS to some degree, a sort of vanilla–chocolate swirl that we’re always trying to figure out…
The VANILLA-CHOCOLATE SWIRL of Sleep Apnea: how do we talk about the thing that’s NOT ONE THING?
And here’s the part we rarely say out loud: The proportions in the swirl can change!
Whaaaaaa?
Truth is: Sleep Apnea is a fluid problem across time and space! We can get different results with changes in body position, jaw posture, altitude, nasal resistance, medications, developmental anatomy, even how aggressively we treat! Sheesh! That’s a lot of MOVING PARTS to contend with, making for a beast that’s not static, but dynamic, contextual, and interactive!
All of this, Life-Fans, brings us to the metric that has launched a thousand arguments…
Ladies and gentlemen, let me present: THE APNEA HYPOPNEA INDEX (AHI).
~ ~ ~ ~ ~
The AHI Problem
The Apnea–Hypopnea Index was never meant to carry the weight we placed on it.
It counts events, that’s all. It does not explain physiology behind them, and it does not necessarily guide treatment mandates or options.
In fact, the AHI can be misleading! Because hypopneas needn’t be designated as one or the other (obstructive vs central), the AHI systematically blends obstructive and central events into a single number, making it possible for two individuals to share an identical AHI and have different mechanisms, different symptoms, different risks, and vastly different treatment needs!
To help unpack this complexity, here on the ISLE, we consider the AHI to be a starting point, not a verdict. We remember that this number tells us that breathing instability exists and quantifies approximately how often. We shy away from using misleading terms like “mild”, “moderate” or “severe” without context, because these terms can’t cut it.
The discussion about why it matters, and what we should do about it?
We called the project Empowered Sleep Apnea, remember?
Well, this is where the EMPOWERMENT comes in…
~ ~ ~ ~ ~
RISK, Finally Said Clearly
The concept of RISK deserves special care, because it’s a hard subject to talk about, and fear distorts conversation faster than almost anything else.
Here is our clear, universe-facing position about how we on the ISLE approach this touchy subject:
Obstructive physiology, especially when occurring frequently and persistently, carries a meaningful long-term risk signal for cardiovascular and metabolic harm. Metrics like the 4% AHI and the newer hypoxic index are helpful indices of how much damage an obstructive pattern of instability is going to be.
Central physiology, in most contexts, carries far less mortality risk and is primarily a driver of symptoms and sleep fragmentation.
RISK is probabilistic, not deterministic, and must be placed in the context of the patient’s known vulnerabilities. Cardiometabolic risk stratification using other indices (labs, carotid intimal medial thickness, etc.) may clarify the discussion about whether RISK is a valid reason to attempt stabilization of a patient’s breathing.
RISK in a given individual is fluid and unfolds over time.
RISK must be discussed honestly, without exaggeration or minimization, and must be used to inform, never to coerce.
In short: RISK matters, and it’s nuanced! Ergo, we treat the conversation about RISK with respect and we do it carefully!
EMPOWERED SLEEP APNEA presents…RISK MANAGEMENT…a page from the “Beautiful Blue Book” explores the tricky notion of discussing RISK!…sometimes it’s hard to talk about! (from McCarty & Stothard 2022)
~ ~ ~ ~ ~
Whew! That was a doozy, but it felt good to get it out of the way. What is Sleep Apnea? It’s unstable breathing during sleep that negatively impacts health, and it has two flavors with MANY MOVING PARTS that can change across time and space.
Life-Fans, if this adds up FOR YOU that no two cases are exactly alike, leading to the realization that there is no one-size-fits-all solution, well, you’re not alone.
That’s exactly what we’re dealing with.
And if there are NO ONE SIZE FITS ALL SOLUTIONS, we suddenly realize why we need our SECOND STAR…
~ ~ ~ ~ ~
Star Two: What Else Could This Be?
The SECOND STAR is our antidote to arrogance. See, every patient with Sleep Apnea has a story behind that label, a set of problems they’ve noted about their sleep/wake experience, something that we call their NARRATIVE.
Here on the ISLE, we’ve learned to prepare folks for the notion that every NARRATIVE may have multiple contributors, and if we stop at the label, we miss out.
This is why the Empowered Sleep Apnea method insists on NARRATIVE-based exploration using the Five Finger Approach(1)— five domains that together form a root-cause map of the sleep–wake system that providers and patients can explore together.
The Five Finger Approach: Orienteering for the Empowerment-Minded!
Circadian alignment
Medications and substances
Medical factors
Psychiatric and psychosocial factors
Primary sleep diagnoses
This structure does something quietly radical:
It gives patients permission to participate in the investigation.
It acknowledges that insomnia, hyperarousal, pain, mood, trauma, reflux, restless legs, circadian misalignment, medication effects, and airway instability often travel together, and that a multi-pronged treatment approach may make sense.
And it restores humility — the recognition that complex systems rarely have single explanations, helping us avoid mistaking correlation for causation, and the temptation to over-titrate our therapy because it’s the one thing we know.
~ ~ ~ ~ ~
Star Three: Why Should We Treat It?
In a siloed, “top-down” management model, treatment decisions are often framed as though the diagnosis itself creates the obligation to intervene, as though crossing a numerical threshold automatically triggers a therapeutic imperative.
A more EMPOWERED approach is to recognize that the diagnosis is just the starting point, a reason to collectively gather our wits and answer the question for ourselves: “WHAT IS SLEEP APNEA?” (see above, if you want a review on how we Empowerees would answer that!)
The point? Diagnosis alone is not a reason to treat.
After we’ve considered other possible contributors to the patient’s NARRATIVE, we see that any decision to stabilize Sleep Apnea is a choice, a collaborative, contextual decision--and it must be grounded in reasons that matter to the person living inside the body.
This is why we use the Five Reasons to Treat(2) as a shared decision framework:
The FIVE REASONS MONUMENT: your discussion at the Coffee Hut awaits…
RISK — for early mortality and moribidity
SNORING — social and relational impact
SLEEP — sleep quality and restoration
WAKE — daytime function, energy, mood
COMORBIDITIES — interaction with other conditions
A key truth that’s often lost: A person may have no strong RISK signal, and still have a completely valid reason to pursue treatment!
Conversely, a person may carry a diagnosis and choose not to treat--and that choice can be ethically sound when made with understanding and agency. See: reasons change; contexts change; bodies change.
That’s why the FIVE REASONS conversation is revisited, not filed away.
See, treatment is not about fixing a number; it’s about helping a person navigate a narrative toward wellness.
~ ~ ~ ~ ~
Why This Matters (To Everyone)
If these three questions sound obvious, let’s ask ourselves why our field still feels so fractured.
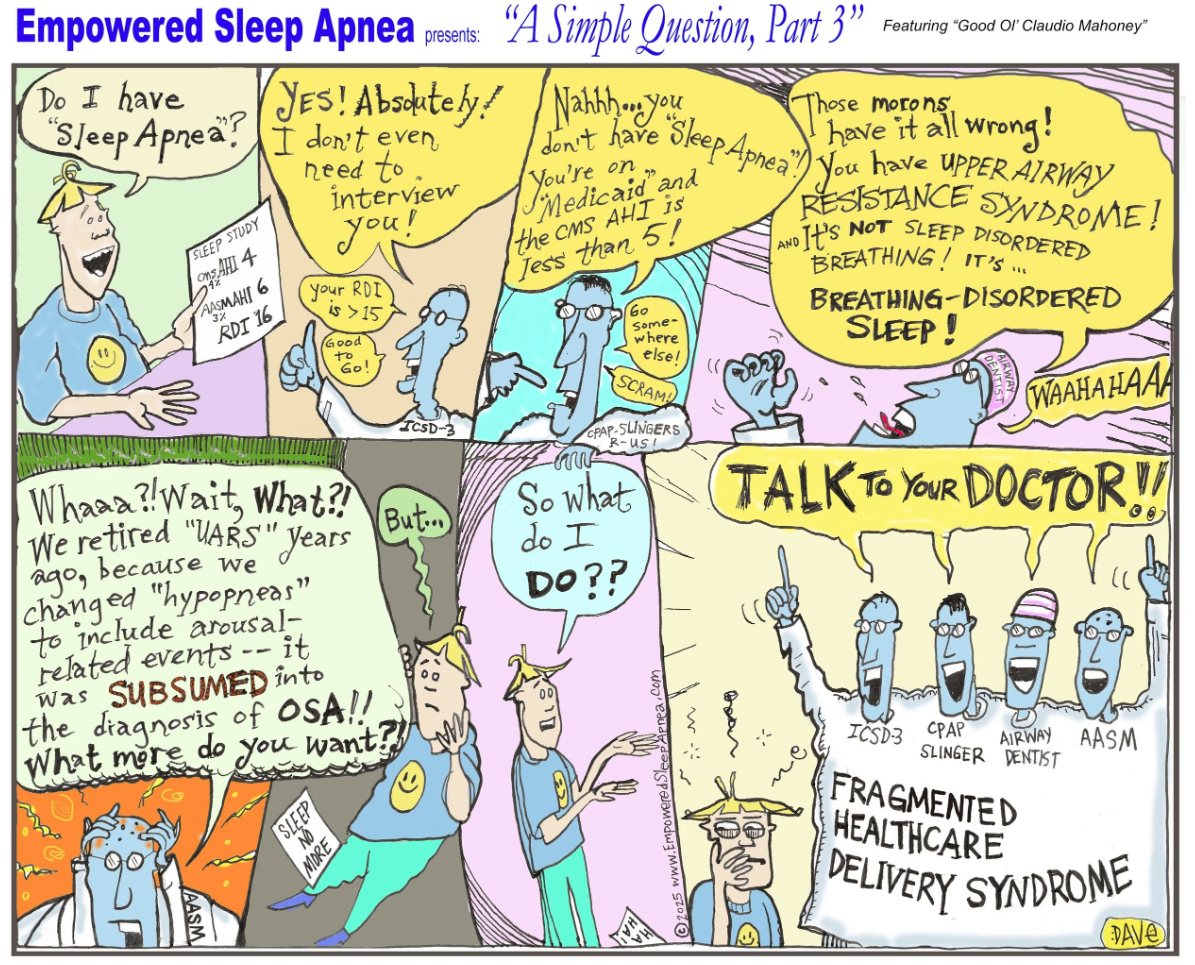
Airway Focused Dentists talk about craniofacial development, autonomic balance during breathing, and “Breathing Disordered Sleep”...ENTs talk about nasal resistance, NOSE scores, and relapse rates after adenotonsillectomy…Pulmonologists talk about the criteria for scoring hypopneas and respiratory effort related arousals and about how “upper airway resistance syndrome” is a moot term, having been subsumed by the diagnosis of Obstructive Sleep Apnea (G47.33).
All are describing the same creature from different angles, and all of them are right.
The problem is to find the language that crosses silos and helps make patients feel whole again.
That, Life-Fans, is the language of EMPOWERMENT.
McCarty, David E. “A Simple Question, Part 3.” Empowered Sleep Apnea cartoon series. Sleep Review, Nov/Dec 2025, p. 26.
~ ~ ~ ~ ~
Wanting Your PHD
We’re in the process of developing a patient-facing document at Rebis, using the complexity deconstruction tools of the Empowered Sleep Apnea project, to assist with the collaborative exploration of these complex issues. We’re calling it the PERSONAL HEALTH DOCUMENT, which we’ve shortened to PHD for obvious reasons of mnemonic snappiness and the innuendo it carries about being smart.
A PHD sounds like a big deal, right? Well, we think it’s a big deal to unpack complexity.
You want your PHD when you’re tired of contradictory explanations, when you sense that something larger is going on, when you want coherence, not coercion.
You want your PHD when you want to be an explorer in your own destiny, not a pawn in someone else’s game.
Happy E’s THREE STARS prepare this ground, making it possible for patients and providers to stand on the same island — the ISLE — looking at the same horizon, speaking a shared language about complexity.
This is not simplification, folks, this is clarity.
These are the ‘Droids we’ve all been looking for.
~ ~ ~ ~ ~
A Declaration from the Mountaintops
So let me say it plainly, without apology: Sleep Apnea is not a disease-state to be conquered, but instead is a complex, evolving landscape to be understood, and every diagnosis deserves humility--an open question about what else might be contributing.
Treatment is not mandatory obedience to a metric, but instead a collaborative response to reasons that matter.
Herein, we’ve toured the THREE STARS of the Empowered Sleep Apnea project, and as I write this, I realize they don’t belong to anyone. They do not belong to Rebis. They do not belong to sleep medicine.
They belong to anyone brave enough to navigate complexity without flattening it.
If we agree on these stars, the silos can play nicely.
If we agree on these stars, patients stop getting lost.
If we agree on these stars, healing becomes possible again.
So I close with a reflection again of my smiling “Happy E”—and the perplexing reason behind his Mona Lisa grin.
Perhaps Happy E smiles not because the journey is easy, but because of the excitement of finally knowing where we’re going.
Kind mojo & steady sailing in the Tall Ship of your choosing,
Dave
David E McCarty MD FAASM
Longmont Colorado
12 Jan 2026
David E McCarty is the co-creator (with Ellen Stothard PhD) of the Empowered Sleep Apnea project (www.EmpoweredSleepApnea.com), and is the Chief Medical officer at Rebis health (www.RebisHealth.org).