What Is Narrative-Based Medicine, and Why Might It Save Us All?
OR: Why Getting the Diagnosis Right is Sometimes the Wrong Question
~ ~ ~ ~ ~
By David E. McCarty MD FAASM (…but you can call me Dave)
20 Jan 2026
~ ~ ~ ~ ~
“Abstraction… becomes a means of arrest far more than a means of advance in thought.
The viciously privative employment of abstract characters and class names is… one of the great original sins of the rationalistic mind.”
—William James, The Meaning of Truth (1909)¹
~ ~ ~ ~ ~
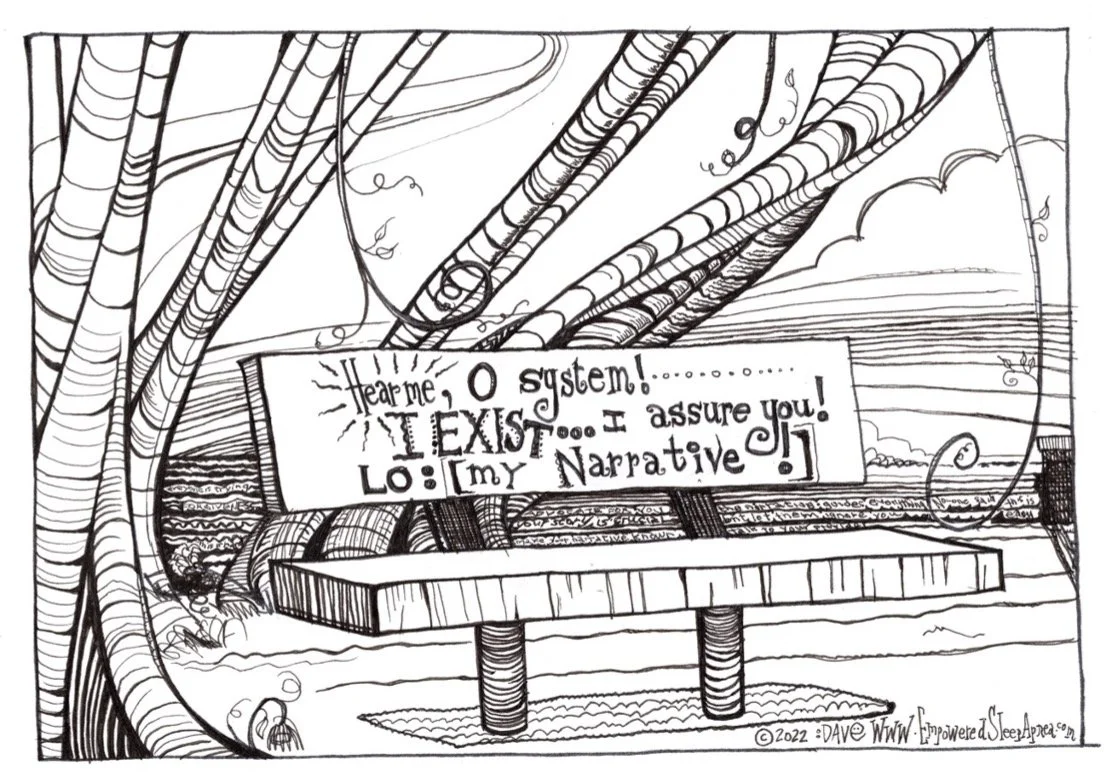
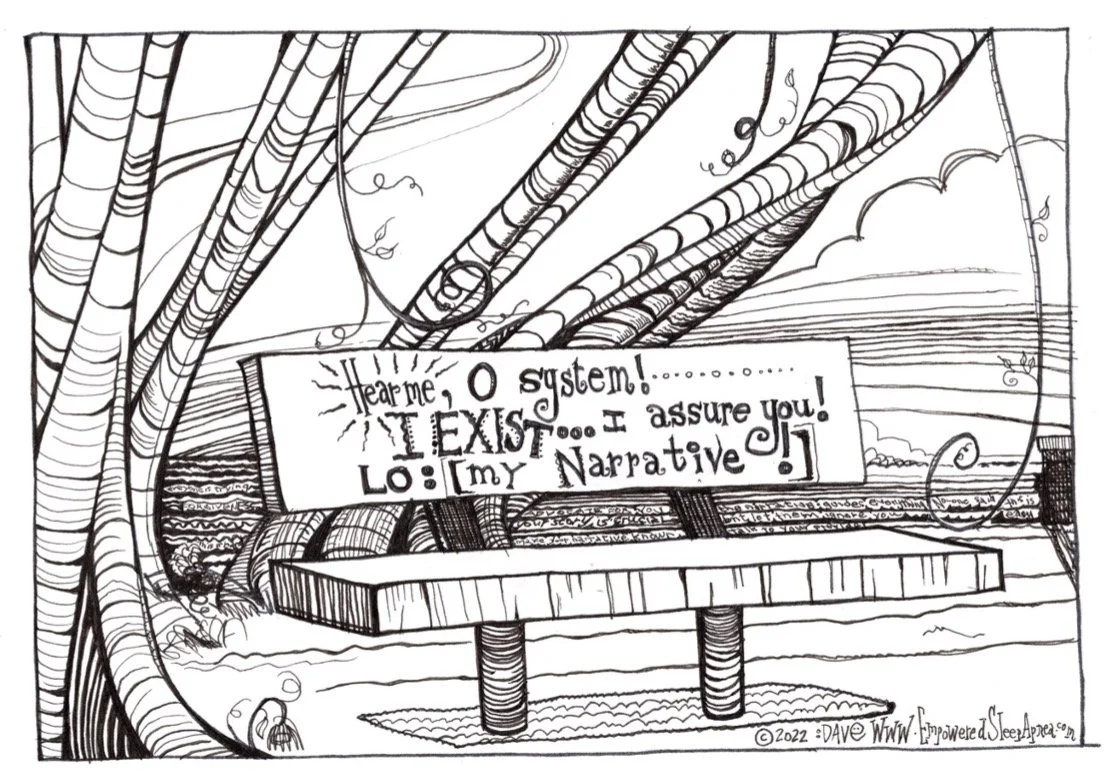
THE CRY OF THE NARRATIVE…hear it roar!
The Naming of Things
Modern medicine is extraordinarily good at naming things.
We have become adept at recognizing patterns, assigning them to categories, and encoding those categories into labels that can be taught, studied, reimbursed, and scaled. This facility with abstraction has enabled astonishing advances. It has allowed science to progress, institutions to coordinate, and healthcare systems to function across distances and disciplines that would otherwise be impossible.
But abstraction has a shadow side.
More than a century ago, the philosopher and psychologist William James warned that abstraction, when mishandled, does not merely simplify reality—it replaces it. When a concept is treated as if it exhausts the thing it names, thought stops moving. Inquiry collapses. The living, breathing phenomenon is reduced to what James called “the naked suggestion of the name abstractly taken.”²
James gave this error a name: vicious abstractionism.
This essay is an attempt to show how vicious abstractionism has quietly embedded itself in modern healthcare, how it manifests as what I will call Label-Based Medicine, and how it produces a wide field of casualties—patients and providers alike—who lose not only clarity, but agency. It is also an attempt to describe an alternative orientation, Narrative-Based Medicine, and to argue that this alternative is not merely kinder or more humane, but ethically necessary in a complex world.
~ ~ ~ ~ ~
The Quiet Collapse of Meaning
Label-Based Medicine begins, almost always, with good intentions.
A patient presents with symptoms. A clinician recognizes a familiar pattern. A diagnosis is made. The diagnosis organizes uncertainty, creates a shared reference point, and suggests a plan. In many cases, this process works well and efficiently. Labels can be powerful tools.
The trouble begins when the label becomes sufficient.
When the diagnosis, once assigned, quietly displaces curiosity rather than sharpening it. When follow-up visits become rituals of confirmation rather than opportunities for renewed inquiry. When the chart tells a story that no longer resembles the person sitting in the room.
At that point, medicine is no longer using labels as tools. It is using them as endpoints.
This is not a failure of intelligence, compassion, or training. It is a predictable structural vulnerability. Abstractions are cognitively efficient. They allow us to manage complexity under time pressure. In an environment increasingly defined by productivity metrics, documentation burdens, and algorithmic pathways, abstraction is rewarded.
But James’s warning applies with full force: abstraction becomes a means of arrest when it replaces lived reality rather than pointing back to it.
Once a label hardens into an identity, it becomes surprisingly difficult to notice when the story underneath it has changed.
McCarty DE. Happy 57th Birthday to the Beast Known as Sleep Apnea! OR: The Monster Has Left the Building. WHAT DO WE DO? Dental Sleep Practice. 5/19/23
~ ~ ~ ~ ~
The Three Foundational Questions
Every clinical encounter, whether explicitly or implicitly, revolves around three foundational questions. When a healthcare system answers these questions coherently, patients feel oriented and empowered. When it answers them inconsistently—or not at all—confusion and suffering multiply.
Those questions are:
What is this?
What else could this be?
Why should we treat it?
Label-Based Medicine tends to collapse these questions into one.
“What is this?” becomes synonymous with the diagnostic label. “Why should we treat it?” is answered by guidelines, risk curves, or reimbursement rules. “What else could this be?” quietly disappears once the label has been assigned.
Narrative-Based Medicine insists on keeping all three questions alive—and in dialogue with one another—over time. In a functioning system, in fact, it safely delivers these three questions into a fourth question, creating a practical loop: “how do we know if it’s working?”
But, as usual, I’m getting ahead of myself. Let’s circle back to the concept of Labels. Specifically: let’s talk about how labels can really screw things up.
~ ~ ~ ~ ~
Casualties of Label-Based Medicine
The casualties of Label-Based Medicine are rarely dramatic. They are quiet, cumulative, and therefore easy to miss.
On the patient side, the casualties are those who no longer feel like active participants in their own care. They comply, but without understanding. They attend visits, but without trust. They sense that something about their lived experience does not quite fit the official explanation, but they lack the language—or the permission—to say so.
Over time, many of these patients disengage. Some become distrustful. Others internalize shame or fear. Still others quietly disappear from care altogether. Their loss is not merely clinical. It is existential. They have lost their sense of authorship over their own story.
On the provider side, the casualties look different but feel eerily similar.
Clinicians working within rigid, label-driven systems often experience a gradual erosion of professional identity. Their curiosity is constrained. Their ethical discomfort accumulates visit by visit as they are asked to prioritize protocols over persons. Burnout and moral injury are frequently framed as individual resilience problems, but they are more accurately understood as signals that the system no longer allows clinicians to think and act as whole moral agents.
Both groups suffer from the same underlying wound: the loss of narrative coherence.
~ ~ ~ ~ ~
Narrative-Based Medicine as an Antidote
Narrative-Based Medicine begins from a different premise.
It holds that human illness unfolds over time, within context, and in relationship. No static category—however useful—can fully capture the lived reality of a person navigating symptoms, fears, tradeoffs, and meaning in the midst of an actual life.
In this orientation, diagnosis is not abolished. It is repositioned.
A diagnosis becomes a provisional hypothesis rather than a final truth. It is something to work with, not something to work under. The guiding question shifts from “What does this person have?” to “What are the ‘moving parts’ involved with this problem, and how is this condition interacting with this person’s life right now?”
This is not sentimentality. It is epistemic humility.
Long before modern complexity science, Aristotle recognized that different domains of knowledge demand different kinds of precision. In matters of ethics and practical action, he argued, truth cannot be derived from rules alone. It requires phronesis—practical wisdom—the ability to judge what is appropriate in a particular circumstance, for a particular person, at a particular time.³
Narrative-Based Medicine is phronetic medicine.
It does not reject general knowledge, but it refuses to mistake generality for sufficiency. It recognizes that in complex biological and social systems, truth is not delivered whole. It emerges through ongoing interpretation. Stories, unlike labels, can evolve as circumstances change. They invite revision rather than closure.
~ ~ ~ ~ ~
Narrative, Ethics, and the Problem of Fragmentation
Modern medical ethics rests on four familiar principles: autonomy, beneficence, non-maleficence, and justice.(4) On paper, these principles appear stable and universal. In practice, they are deeply dependent on how meaning is constructed within the clinical encounter.
Autonomy without narrative becomes consent without understanding.
Beneficence without narrative becomes intervention without relevance.
Non-maleficence without narrative becomes harm avoidance detached from healing.
Justice without narrative becomes efficiency stripped of fairness.
Ethical principles cannot be applied wisely without a coherent account of what matters to the person whose life is being affected. Without narrative, ethics becomes procedural rather than moral.
In this light, we blink our eyes and realize that the ethical failures we attribute to individuals are often failures of systems.
Well, folks…it’s time we started talking about that!
~ ~ ~ ~ ~
Complexity, Systems, and Shared Meaning
Back in the early 2000’s, Gen. Stanley McChrystal (U.S. Army, retired) came to a similar realization in a very different context. Leading military operations in Iraq, he found that traditional command-and-control structures were incapable of responding to a fast-moving, adaptive environment. As he revealed in his bestselling book Team of Teams: New Rules of Engagement for a Complex World, the solution was not tighter control, but shared consciousness—a common understanding of the problem space—and lateral connectivity, the ability of teams to coordinate and act without waiting for top-down permission.(5)
Healthcare increasingly resembles the environment McChrystal described.
Knowledge is fragmented across silos. Patients move between specialties carrying incompatible explanations. Providers optimize locally while coherence collapses globally. The result is a system that feels unintelligible to those who must navigate it.
Interestingly, one of the most successful large-scale experiments in managing human complexity emerged not from medicine or the military, but from an amusement park.
~ ~ ~ ~ ~
Disney, Design, and Ethical Environments
Walt Disney understood that systems designed for humans must be oriented around shared meaning. As I explored in a recent essay series, Disneyland functioned not merely because of attractions, but because of a unifying ethic operationalized through simple, shared principles—ideas he called the four keys: SAFETY, COURTESY, SHOW, and EFFICIENCY.
These principles were not slogans. They were moral priorities embedded in daily decision-making at every level of the organization.
When examined closely, they map uncannily onto the foundations of medical ethics. Safety aligns with non-maleficence. Courtesy with respect for autonomy. Show with beneficence made visible. Efficiency with justice embodied.
Disney’s insight was not about entertainment. It was about designing environments that support humane action under conditions of complexity.
~ ~ ~ ~ ~
Narrative-Driven Tools and the Rebis Model
Narrative-Based Medicine is not merely a philosophy; it is a practice discipline, and like any discipline that hopes to survive contact with the real world, it requires infrastructure.
At Rebis Health, this infrastructure takes the form of narrative-driven complexity deconstruction tools designed to help patients and clinicians think together in the presence of uncertainty, rather than rushing toward premature closure. These tools exist to keep the three foundational questions alive—What is this? What else could it be? Why should we intervene?—not as a linear checklist, but as an ongoing, iterative conversation that unfolds over time.
Central to this approach is the recognition that the conditions we label—Sleep Apnea chief among them—are not singular entities but dynamic constellations of conditions, interacting across biological, psychological, social, and temporal domains. We embrace a systematic trans-diagnostic strategy using the Five Finger Approach (6) providing a shared map for exploring competing diagnoses without collapsing the story too quickly into a single explanatory frame. By deliberately scanning circadian factors, medications and substances, medical conditions, psychiatric and psychosocial influences, and primary sleep disorders, clinicians and patients are invited into a process of joint discovery that preserves humility and resists the cognitive lure of early closure.
Similarly, the Five Reasons to Treat (7) offers a narrative scaffold for answering not whether a diagnosis exists, but whether intervention is meaningful for the person living inside the diagnosis. Rather than assuming that treatment is obligatory once a label has been applied, this framework re-centers the conversation on reasons that matter—risk, sleep quality, daytime function, snoring and relational impact, and the interaction with comorbid conditions. In doing so, it restores agency to the patient and ethical clarity to the clinician, ensuring that intervention remains a choice grounded in values, not a reflex driven by metrics alone.
Once a patient-centered treatment mandate is established, Sleep Apnea can be broken down into its MANY MOVING PARTS (7), enabling a clear-eyed method of addressing one (or more) individual components (functional, physiologic, anatomic) that contribute to this complex disorder.
Taken together, these tools do not replace clinical expertise; they humanize it. They allow clinicians to remain curious without becoming overwhelmed by complexity, and they allow patients to participate as co-authors of their care rather than passive recipients of decisions made elsewhere. Most importantly, they create a shared language capable of restoring coherence in a fragmented healthcare landscape—one conversation at a time.
~ ~ ~ ~ ~
Conclusion: Keeping the Story Alive
Label-Based Medicine did not arise from malice. It arose from efficiency under pressure. But efficiency without wisdom eventually undermines the very goals it seeks to serve.
William James’s warning remains painfully relevant. When abstraction becomes an endpoint rather than a tool, it arrests thought. It freezes systems that must remain adaptive.
Narrative-Based Medicine offers a way forward that is neither nostalgic nor naïve. It does not ask us to abandon science, but to place it back into relationship with lived experience. It reminds us that diagnoses are tools, not identities, and that healing is not a transaction but a story unfolding over time.
In the end, this is not an argument against labels…
…it is an argument for seeing past them…
…for remembering that the person is still alive…
…that the story is still in motion…
…and that the ethical work of medicine is never finished.
Hear me, O System! I exist…I assure you! Lo: MY NARRATIVE!
Kind mojo,
Dave
David E. McCarty MD FAASM
Longmont, Colorado
20 January 2026
David E McCarty is the Chief Medical Officer of Rebis Health, and the co-creator (with Ellen Stothard, PhD) of the Empowered Sleep Apnea project.
It’s not just a HAIKU…it’s a revelation! The Cry of the NARRATIVE…first appeared in McCarty & Stothard (2022) (7)
~ ~ ~ ~ ~
References
James, W. The Meaning of Truth: A Sequel to “Pragmatism.” New York: Longmans, Green, & Co., 1909.
Ibid., Chapter XIII, “Abstractionism and ‘Relativismus.’”
Aristotle. Nicomachean Ethics, Book VI.
Beauchamp, T. L., and Childress, J. F. Principles of Biomedical Ethics. 1st ed. Oxford University Press, 1979.
McChrystal, S., Collins, T., Silverman, D., & Fussell, C. Team of Teams: New Rules of Engagement for a Complex World. New York: Penguin, 2015.