Good Trouble in the Dental Chair
OR: Reading the AADSM Consensus Through the Language of Empowerment
~ ~ ~ ~ ~
By David E. McCarty, MD, FAASM
(…but you can call me Dave)
31 January 2026
~ ~ ~ ~ ~
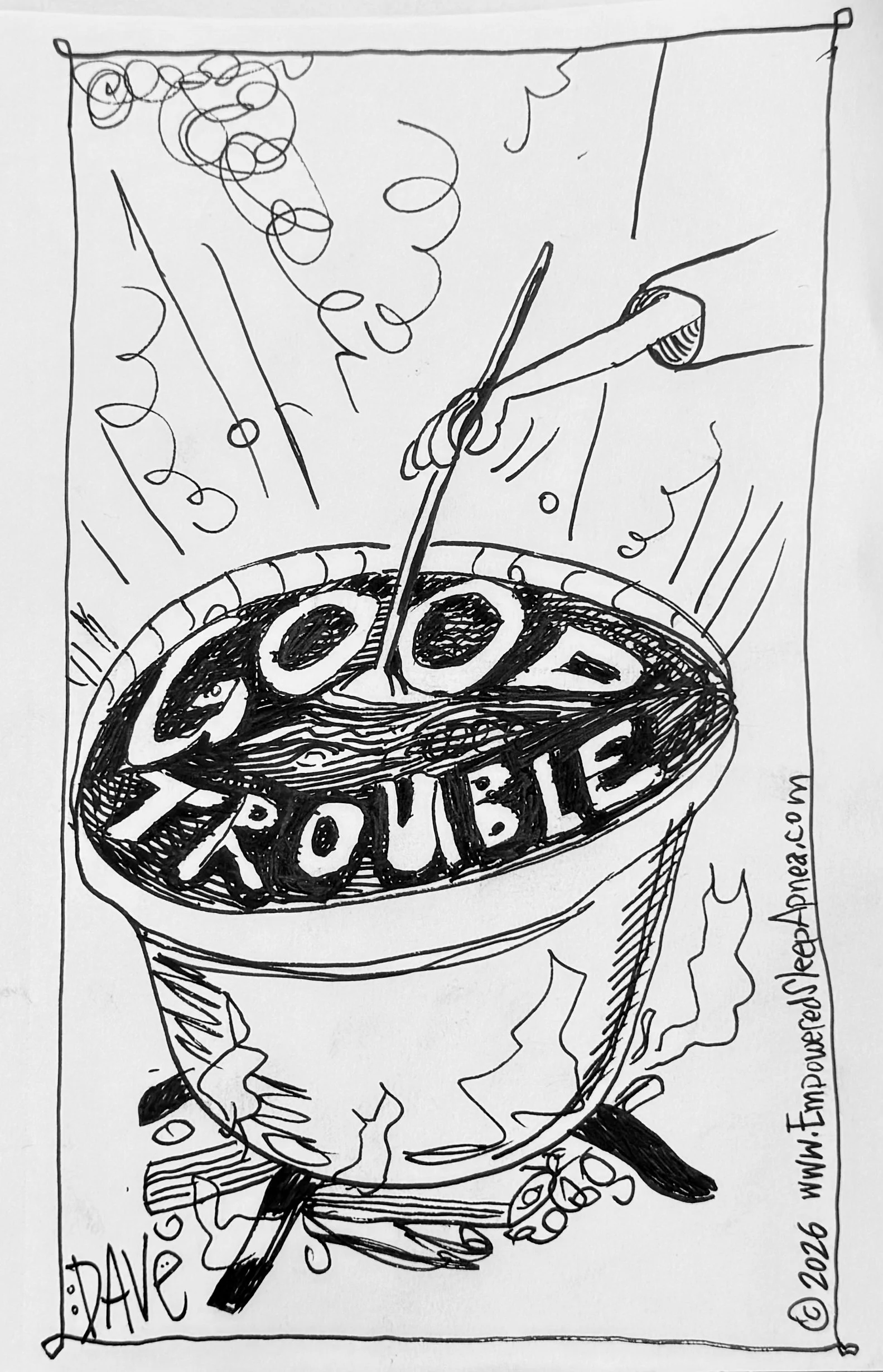
“Get in good trouble. Necessary trouble.”
--John Lewis [1]
~ ~ ~ ~ ~
Let’s stir up some Good Trouble!
“Good Trouble”
There is a particular kind of paper that appears at moments of quiet transition in a field.
It doesn’t arrive waving a flag or declaring a revolution. It arrives instead with careful language, consensus tables, color-coded caution, and an almost palpable effort not to overclaim. These papers are quietly radical in their deliberate honesty. They don’t provoke for sport. They don’t posture. They do something harder: they ask us to slow down and look again.
John Lewis once called this kind of stance good trouble—the necessary kind. Not the loud kind. Not the scorched-earth kind. The kind that emerges when people take their work seriously enough to let it outgrow its old language.
In complex systems, that kind of honesty is often the first signal that something deeper is shifting.
The 2024–2026 American Academy of Dental Sleep Medicine (AADSM) consensus on emerging dental therapies for sleep disorders [2] is one of those papers. It deserves to be read slowly, generously, and—most importantly—without the usual reflex to ask whether it delivers a new heroic therapy that’ll save the day. That reflex, I would argue, is precisely the habit this paper is quietly leaving behind.
So let me begin here, clearly and without irony:
Good job, folks!
This consensus does several things right—bravely right—in a scientific culture that often rewards certainty over humility. And it is precisely because it does so many things right that it opens the door to a deeper conversation about how we talk about Sleep Apnea, dentistry, and healing itself.
What follows is not a rebuttal or critique in the usual sense. Think of it instead as an act of translation—an attempt to read this careful, disciplined document through what I’ll call the language of empowerment, and to see what new questions emerge when we do.
Climb aboard the Blue Balloon…let’s take a look!!
Welcome aboard! Empowerment changes everything…
~ ~ ~ ~ ~
What the Paper Gets Right (and Why That Matters)
First, credit where credit is due.
The AADSM consensus resists hype at a moment when hype would be easy. In an era of social-media dentistry, laser enthusiasm, and epigenetic nudges, this group of authors repeatedly says some version of: slow down. No emerging dental therapy, they conclude, meets criteria as a first-line monotherapy for obstructive sleep apnea or snoring. That sentence alone probably disappointed more than a few conference exhibitors.
Second, the paper explicitly acknowledges what many consensus documents only imply: AHI is a weak proxy for lived experience. The authors note—correctly—that the apnea–hypopnea index correlates poorly with quality of life, long-term outcomes, and functional health. They name the absence of consistent patient-centered outcomes. They point toward physiology, sleep architecture, circadian rhythm, and neurocognitive function as under-measured domains.
That admission matters. It signals epistemic humility. It tells us the authors are not mistaking the map for the terrain.
Third, the paper names complexity without trying to crush it. Pediatric heterogeneity, developmental timing, COMISA (comorbid insomnia and sleep apnea), circadian misalignment, and adherence challenges are not treated as footnotes. They are treated as structural features of the problem.
In other words, this is not a paper written by people who believe the beast we all go around calling Sleep Apnea is a simple plumbing problem.
And yet…
~ ~ ~ ~ ~
The Question Beneath the Questions
Despite all of this, the paper is organized around a single, largely unquestioned axis:
Can this therapy function as a first-line monotherapy at the population level?
Everything flows from that question—the color codes, the red boxes, the yellow uncertainty, and the conspicuous absence of green.
From the standpoint of the Empowered Sleep Apnea project, this is not wrong…it’s just…narrow. And in complex systems, narrow questions quietly predetermine narrow answers.
Monotherapy is a powerful idea. It implies clarity, hierarchy, and replacement. One thing stands in for another! One intervention solves the problem! One metric defines success.
One size fits all. Huzzah!!
Cartoon originally in: There is No OSFA: How the Many Moving Parts of Sleep Apnea Demands Precision Medicine. Dental Sleep Practice. 2023;10(1) 18-20 [3]
~ ~ ~ ~ ~
Except, of course, it doesn’t work like that.
Everybody now knows that Sleep Apnea—particularly as it shows up in real human beings—is not a single thing waiting to be solved. It is a syndrome of converging constraints: anatomy, arousal threshold, ventilatory control, sleep timing, mental health, medication effects, life context, and meaning.
When we ask whether a dental therapy can replace PAP or mandibular advancement devices, we are already assuming the problem is singular. The AADSM consensus itself repeatedly demonstrates that it is not.
From an empowerment perspective, the more interesting question is different:
What problem is this intervention actually helping this person solve, right now?
Empowerment does not invalidate the consensus.
It completes it.
~ ~ ~ ~ ~
AHI: Named, Acknowledged, and (sigh) Still Enthroned
One of the most revealing tensions in the paper is its relationship with the primary metric of Sleep Apnea severity: the apnea–hypopnea index (AHI).
On the one hand, the authors are admirably clear-eyed about its limitations. They cite evidence showing poor correlation with outcomes patients actually care about. They acknowledge the absence of standardized snoring metrics and the underuse of validated functional scales.
On the other hand, AHI remains the gravitational center of the evaluative framework. Evidence is graded, therapies are categorized, and conclusions are drawn largely through its lens.
This is not hypocrisy; it is our heritage.
Sleep medicine has built its shared language around AHI for decades. Even when we know a language is incomplete, abandoning it requires not just insight, but replacement.
The language of empowerment does not suggest throwing AHI away. It suggests de-centering it—placing it alongside other domains of healing rather than above them.
When a patient says, “I’m sleeping better, thinking more clearly, my blood pressure medications were reduced, and I no longer dread bedtime,” the empowered response still notes the residual AHI. But it doesn’t stop there. It asks what that breathing pattern means for this person, at this time, and what “moving parts” might actually matter, when we attempt to stabilize it.
~ ~ ~ ~ ~
Pediatrics, Time, and the Tyranny of Permanence
Nowhere is the monotherapy frame more limiting than in pediatrics.
The consensus carefully notes that orthodontic and myofunctional interventions may show benefit until adulthood, and then quietly treats that conditionality as a weakness. From a linear, adult-centric view of disease, that makes sense. If a therapy does not permanently eliminate risk, it is suspect.
But children do not live in linear time. They live in developmental time.
From an empowerment lens, early interventions are not expected to “cure” adult disease. They are expected to shift trajectories—to reduce constraint, expand possibility, and support healthy growth.
A child who sleeps, breathes, and develops differently between ages four and twelve is not the same biological system at eighteen, regardless of what their adult AHI eventually becomes.
The real question is not whether early dental interventions create permanent immunity from a diagnostic label. It is whether they create room—room for balanced naso-diaphragmatic breathing, healthier sleep architecture, neurocognitive development, emotional regulation, and relational stability during critical windows.
Our current evidence language struggles to name that kind of success.
~ ~ ~ ~ ~
Dentistry as “Helper”… or as Collaborative Participant?
Throughout the paper, dentistry is described as a contributor, supporter, screener, or adjunct. This is not dismissive. It reflects professional boundaries and respect for multidisciplinary care.
And yet, from an Empowered Sleep Apnea perspective, something important is hiding in plain sight.
Dentists are among the few clinicians who routinely observe craniofacial structure, oral function, breathing patterns, bruxism, airway crowding, and behavioral habits tied to sleep. They see patients early, repeatedly, and outside of crisis moments.
In complex systems, those observers are not junior partners. They are sentinels with a unique lens.
We have moved past the era where a sleep physician could “order” a mandibular advancement device from a dentist like pressing a button on a vending machine. The nuance of device selection, risk, failure modes, and the appropriateness of expansive orthodontic techniques demands imaging, expertise, deep clinical judgment, and patient involvement.
The language of empowerment does not ask airway-focused dentistry to replace sleep medicine. It asks us to acknowledge that airway health, sleep behavior, and physiology co-evolve—and that no single discipline owns the whole story.
Let’s be honest: this problem is too big for one silo.
~ ~ ~ ~ ~
Adjunctive is Not a Dirty Word
One of the most quietly radical moves in the consensus is its normalization of adjunctive, individualized, and context-dependent interventions.
In traditional evidence hierarchies, “adjunctive” can sound like failure. From an empowerment perspective, it sounds like honesty.
Complex problems are rarely solved by single tools. They are managed by toolkits—revisited over time and adapted to changing circumstances.
When a dental intervention helps a patient tolerate PAP, remain engaged in care, reduce arousal burden, or reclaim agency, that is not marginal success. It is foundational.
Our inherited language struggles to honor that.
~ ~ ~ ~ ~
A Different Language for Success
What if, instead of first-line versus adjunctive, we organized our thinking around different questions?
Which moving parts of Sleep Apnea matter most for this patient? Which interventions engage those parts? And how will we know when we’ve achieved the patient’s goals?
The AADSM consensus already contains the raw material for this reframing. It simply lacks the language to name it.
~ ~ ~ ~ ~
Ending Where the Paper Already Points
The authors conclude, appropriately, with caution, with something that might be misinterpreted as a final pronouncement of value: no emerging dental therapy is ready to replace established first-line treatments and more research is needed.
Broader outcome measures should be developed, and collaboration matters.
All of that is true.
But something else is also true, and the paper hints at it repeatedly without quite saying it aloud: our greatest limitation is no longer a lack of interventions. It is a lack of language.
We have tools that shape development, influence physiology, support adherence, and alter lived experience. What we lack is a shared way to talk about success that honors complexity without abandoning rigor.
If the Empowered Sleep Apnea project adds anything here, it is not a new therapy. It is an invitation—to speak differently about healing, to ask better questions, and to recognize that empowerment is not the opposite of evidence.
It is what evidence looks like when it finally meets real human lives.
That kind of trouble—the quiet, necessary kind—is worth stirring up!
Kind mojo,
Dave
David E McCarty MD FAASM
Boulder, Colorado
31 January 2026
David E McCarty is the co-creator (with Ellen Stothard, PhD) of the Empowered Sleep Apnea project (www.EmpoweredSleepApnea.com) and the Chief Medical Officer of Rebis Health (www.RebisHealth.org).
~ ~ ~ ~ ~
References
Lewis JR. Across That Bridge: Life Lessons and a Vision for Change. New York: Hyperion; 2012.