KPAP: THE WRITING IS ON THE WALL
Or: How an “Upside-Down” Pressure Strategy Might Just Save Us All
By David E McCarty MD FAASM (…but you can call me Dave)
30 December 2025
~ ~ ~ ~ ~
“The real voyage of discovery consists not in seeking new landscapes, but in having new eyes.”
Marcel Proust
in: À la recherche du temps perdu (In Search of Lost Time)
Volume V: La Prisonnière (1923).
~ ~ ~ ~ ~
Ready or not…KPAP is coming!!! :O)
I’ve been paying close attention to the work of my friend Dr. Bill Noah over the last couple of years, because in my bones, in my Spidey-Sense intuition, I know he’s onto something. After reading his recent invited editorial to Sleep & Breathing, it’s time to share why.
Because for a long time now, many of us have been living with a nagging, half-formed thought we didn’t quite know how to say out loud:
What if too much pressure isn’t…um…benign?
Walk with me here, but what if much of the instability we see on therapy (shabby compliance, unstable AHI metrics, unfavorable subjective responses) isn’t a mysterious patient failure, but a predictable physiologic response to how we deliver pressure in the first place?
What if we’ve been mistaking engineering enthusiasm for clinical wisdom?
I like Bill’s paper, because it doesn’t shout or grandstand. In my view, it does something far more disruptive: it calmly walks us back through forty years of PAP history and asks whether the assumptions we’ve been building on were ever as solid as we believed. In doing so, it gives the clinical syndrome I’ve been calling pressure toxicity a legitimate scientific lineage.
So how did we get here?
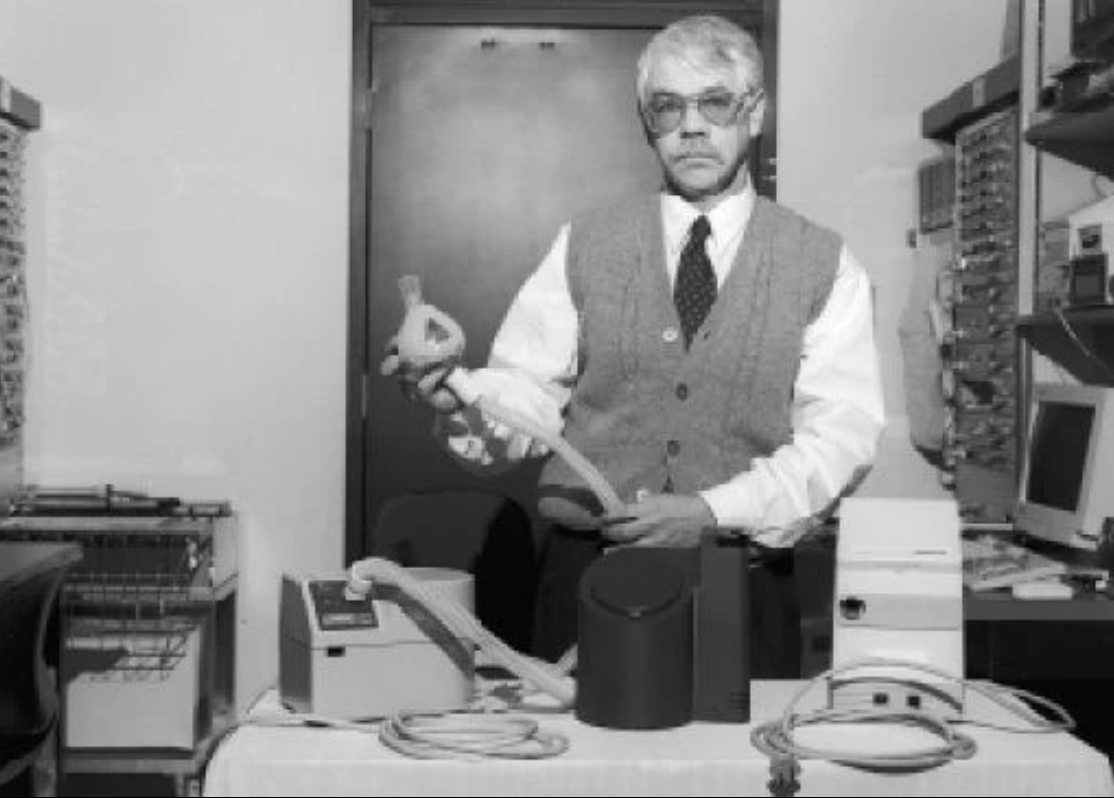
Cue theremin sound effects as the screen fades to a scratchy 16mm film showing us “the old days…”
~ ~ ~ ~ ~
Pressure Toxicity! it’s out there!!
~ ~ ~ ~ ~
From CONTINUOUS to CONSTANT to “MORE”—oh my!
CPAP was never meant to be elegant.
It was meant to be sufficient, you know? Colin Sullivan’s original concept was simple: maintain airway pressure above atmospheric levels across the respiratory cycle to counteract collapse driven by negative inspiratory pressures.
Early devices were crude by today’s standards—the first devices had removable valves to regulate different pressures. On these early machines, pressures fluctuated over the respiratory cycle. Inspiratory pressure drops happened. And yet—remarkably—airways stayed open and patients improved.
In 1980, “CPAP” was a cobbled-together vision created by Colin Sullivan, a nasal mask hooked up to a paint compressor motor…how times have changed!
Then the engineers started scratching their heads. Somewhere along the way, “continuous” quietly morphed into “constant.” Then constant became responsive. Responsive became anticipatory. Anticipatory became aggressive.
Suddenly, we’ve got all kinds of new add-ons to help deal with the sense that exhaling against too much pressure is uncomfortable! Pressure support features proliferated. Compensation algorithms like “expiratory pressure relief” multiplied. Patients get “graduated” to oronasal interfaces because of excessive mouth leak with a nasal mask. The machine learned to chase every perceived instability.
And, meanwhile, we clinicians largely assumed that if some pressure was good, more precision—and often more pressure—must be better!
Dr. Noah does something almost heretical here, and here’s why this paper deserves so much air time, in my opinion:
Dr. Noah had the gall to ask for evidence!
What emerges from that simple question is uncomfortable, because the truth is we’ve collectively added layers of pressure manipulation without clear proof of benefit, while slowly and painfully cataloguing accumulating signals for harm: increased leak, aerophagia, discomfort, and—most notably—treatment-emergent central sleep apnea (TECSA).
~ ~ ~ ~ ~
CSA is Not One Thing
This is where the conversation needs to grow up.
As I’ve recently reviewed in a shockingly sparky cartoon-essay combo, Central sleep apnea physiology has many moving parts! Loop gain. CO₂ reserve. Cardiac status. Chemoreceptor sensitivity. Sleep stage. Jaw posture. Source of periodic arousals. You don’t “fix” that with force; you jiggle the handle and figure out which part needs stabilizing. When we see it as a quest for physiologic coherence instead of compliance, we see a different journey.
THE GORDIAN KNOT OF CENTRAL SLEEP APNE: Care to take a turn in unraveling it?
What Bill’s work makes painfully clear is that CSA is often iatrogenic—not because PAP is bad, but because how we apply pressure matters. Increasing inspiratory pressure above expiratory pressure has the tendency to wash out CO₂, amplify ventilatory instability, and tip vulnerable systems into oscillation. This is especially true at moderate-to-high elevation, like we see here in the Front Range in Colorado.
Take that complexity, and sprinkle in real-world posture and position changes: the open-mouth breathing position with or without supine positioning, unintentional leaks causing worsening CO2 washout and increased minute ventilation.
Quietly, insidiously, the machine is “winning” while the patient is unraveling. And then we call it noncompliance.
Yay, team!
~ ~ ~ ~ ~
Revisiting Risk and Benefit
For decades, the risk–benefit conversation around CPAP has been framed in relatively simple terms. Untreated obstructive sleep apnea carries well-documented risks, and positive airway pressure reliably reduces upper-airway collapse. In that context, escalation of pressure has often been treated as a largely benign means to a clearly defined end.
But as our understanding of sleep-disordered breathing has matured, so too must the way we talk about risk.
It is increasingly clear that CPAP is not a binary intervention—on or off, working or failing—but a dose-dependent physiologic exposure. Pressure alters lung volumes, ventilatory drive, intrathoracic pressures, sleep architecture, and carbon dioxide homeostasis. These effects are not uniform across patients, nor are they without consequence.
Recent work suggests that higher pressure strategies may, in some individuals, destabilize breathing, promote treatment-emergent central sleep apnea, increase unintentional leak, and—under certain conditions—be associated with adverse inflammatory and cardiovascular signals. At the same time, the device-reported metrics we often rely on to declare success become less reliable precisely when leaks and over-ventilation are present.
Taken together, these observations argue for a more nuanced risk–benefit discussion—one that acknowledges both the undeniable benefits of PAP therapy and the possibility that more is not always better.
In this emerging frame, the primary therapeutic goal shifts subtly but importantly: from the pursuit of numerical perfection toward the pursuit of physiologic stability and coherence. Success is no longer defined solely by adherence or machine-reported indices, but by whether treatment supports stable breathing, restorative sleep, tolerability, and patient-centered goals over time.
This does not represent a retreat from therapy, but a maturation of it. It asks us to pair technological capability with clinical restraint, and to engage patients as partners in deciding when the marginal gains of additional pressure may be outweighed by unintended costs.
In other words, the question is no longer simply “Can we eliminate events?”
Dr. Noah is asking all of us to ask “At what point does eliminating the last events begin to cost more than it gives?”
~ ~ ~ ~ ~
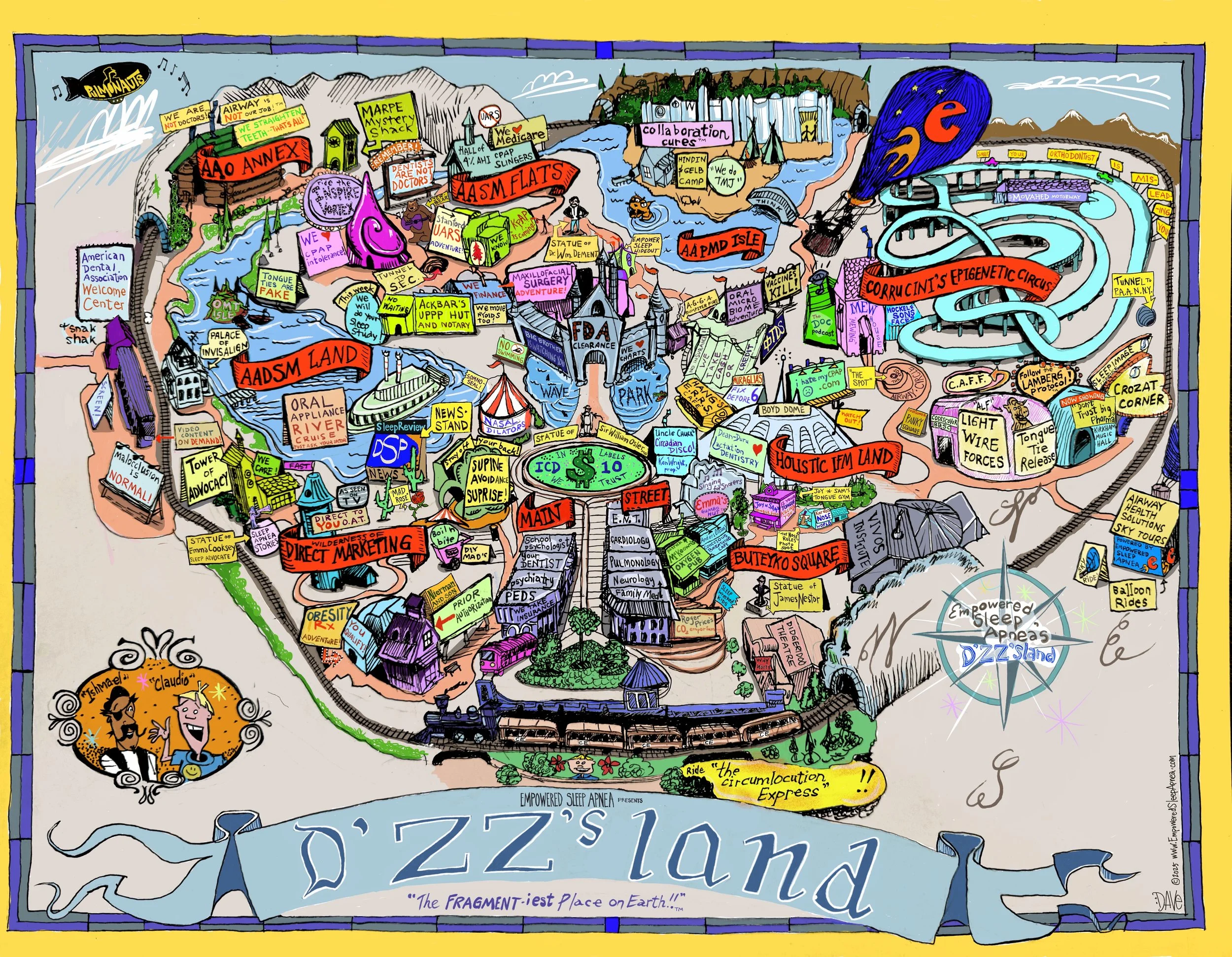
BEHOLD! The Fragmentiest Place On Earth (TM) LOL! :)
~ ~ ~ ~ ~
The Writing on the Wall
In my cartoon universe of our fractured Sleep Medicine healthcare landscape—"The Fragmentiest Place on Earth ™”—walls are where institutions post laminated truths. But walls are also where reality pushes back.
In the cartoon, you might notice that there’s a small figure over in the AASM section of the park, loitering outside one of the buildings, spray-painting a message that isn’t a slogan so much as a warning:
K.P.A.P. is coming.
the writing is on the wall…
…it’s up to us to read it :)
Maybe not as a savior, Life-Fans, perhaps that’s too dramatic…but I surely see KPAP as a messenger we all need to be listening to…
Long before medicine codifies change, it often appears first as graffiti—quiet, unofficial, impossible to unsee once you notice it. Bill Noah’s work doesn’t demand that we abandon PAP. It asks us to grow up in how we use it.
To acknowledge that too much pressure can be toxic, that CSA is often something we create when we stop listening, and that the true measure of success is not whether the machine is happy, but whether the patient is stable, sleeping, and whole.
The writing really is on the wall.
The only question now is whether we’re willing to read it.
Thank you, Dr. Bill Noah, for your relentless pursuit of the truth, and Happy New Year to all!
Kind mojo,
Dave
David E McCarty MD, FAASM
Longmont, Colorado
30 December 2025
References/Further Edification
Sullivan, C. E., Issa, F. G., Berthon-Jones, M., & Eves, L. (1981). Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. The Lancet, 317(8225), 862–865. doi:10.1016/S0140-6736(81)92140-1
Noah WH. Using CPAP to treat OSA: Is it time to reverse 30 years of understanding and engineering? Sleep and Breathing. 2026;30:16. doi:10.1007/s11325-025-03562-2.
Noah WH, Messineo L, Hete B, et al. Treatment-emergent central sleep apnea resolves with lower inspiratory pressure. Journal of Clinical Sleep Medicine. 2024;21(3):559–564.
Simmons JD, et al. 0634 A Remote-Patient-Monitoring System Using FDA-Cleared Wearable Technology for OSA Management Overcomes Deficiencies Found in PAP AHI RPM Data. SLEEP 2025 Abstract #0634.
Peker Y, Celik Y, Behboudi A, et al. CPAP may promote an endothelial inflammatory milieu in sleep apnoea after coronary revascularization.
eBioMedicine. 2024;101:105015. doi:10.1016/j.ebiom.2024.105015.Richard M, Fresnel E, Mallet J-P, et al. Performances of Auto-CPAP Devices Under Real-Life Leak Patterns: A High-Fidelity Modeling Approach.Archivos de Bronconeumología. 2025;61:311–314. doi:10.1016/j.arbres.2025.01.008.
Iftikhar IH, BaHammam A, Jahrami H, Ioachimescu O. Accuracy of residual respiratory event detection by CPAPs: A meta-analysis.
Sleep and Breathing. 2023;27:1759–1768.